Introduction:
Covid-19 was a challenge like no other. With a world connected like never before and intertwined economies the virus spread like wildfire across the globe. However, as they say, every new challenge is an opportunity to create a better and more secure tomorrow. Devastating as it was, the aftermath of Covid-19 toes the line. The pandemic saw academics, scientific community, medical professionals and data scientists come together to assess unique methods that are rapid and secure to tackle the crisis with virtual health services. Data sharing, a key component in creating solutions was incentivised along with model training and testing without the hurdles of conventional collaborations. Healthcare providers and researchers focused on addressing the challenges of meeting the critical clinical needs created by the crisis, with remarkable results.
As per the article Federated learning for predicting clinical outcomes in patients with COVID-19 published in Nature Medicine “The pandemic has emphasized the need to expeditiously conduct data collaborations that empower the clinical and scientific communities when responding to rapidly evolving and widespread global challenges.”
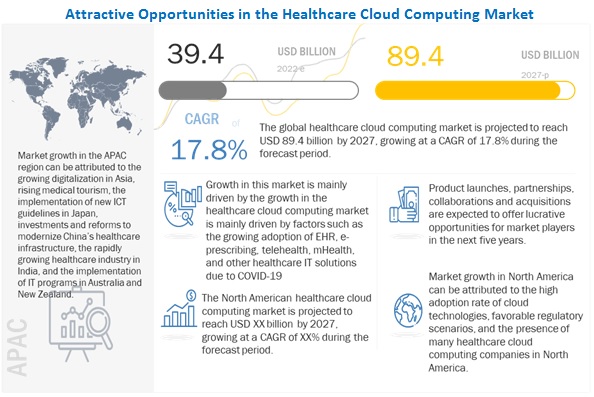
Since the Covid-19 outbreak, Investment in digital health has skyrocketed, Venture Capitalists are queueing up to invest in the digital healthcare more than ever before. Thus providing the impetus for further innovation. Artificial Intelligence(AI) is another sector which proves to be a strong pillar of support for the Data Scientists, Academicians, Healthcare Professionals and Regulatory Authorities.
Regulatory Changes:
There was a slew of regulatory changes brought in by the US Government to tackle the pandemic and ensure faster care to the patients. The regulations aim to improve the safety of the healthcare professionals. We look at some of the blanket waivers brought in during the Pandemic:
Emergency Medical Treatment & Labor Act (EMTALA): By waiving off the section 1867(a) of the act, it facilitates hospitals to screen patients offsite. This helps to prevent the spread of Covid-19.
Telemedicine: By waiving of certain sections related to 42 CFR, virtual health services became accessible to patients through an agreement with offsite hospital.
Quality Assurance and Performance Improvement (QAPI): This enabled the healthcare facilities to develop, implement, maintain and evaluate an effective and exhaustive data-driven QAPI. Thereby the hospital can solely focus on treating patients during COVID-19.
Electronic Case Reporting (eCR): The automated generation and dissemination of case reports from the electronic health record (EHR) to public healthcare agencies makes disease reporting faster and easier. It moves data securely and seamlessly—from the EHR at the point of care, to data systems at state, territorial, and local agencies. This also allows public health to provide information back to healthcare professionals. The timely data sharing provides a real time picture of COVID-19 to support outbreak management.
To cover the entire set of regulatory changes and waivers is beyond the scope of this article. For more details do go through the link.
Trends during the Pandemic:
The pandemic brought forth the need for an alternative method of healthcare and allied health services. While this blog is being written, digital technologies are being harnessed to help prepare for future challenges.
Dissemination of information from credible sources – IT platforms were widely used by regulatory authorities to deal with the misinformation and educate the masses about Covid-19. WHO rolled out the ‘Stop the Spread’ campaign across platforms. They also rolled out another campaign within the campaign Playbook to tackle the wastage of resources. The aim is to document and share innovative and good vaccination practices to educate the countries and communities at large.
One sector which emerged as the sunshine sector during the Pandemic is the Telehealth. With regulatory changes which facilitated the accessibility becoming permanent like for eg; the reimbursable telehealth codes for the 2021 fees schedule for physicians, the sector is witnessing an expansion in terms of services that it can offer.
According to a report by McKinsey, Tele Health services has increased 38 times since pre Covid days. The report mentions that consumers continue to view telehealth as an important modality for their future care needs. But the view varies widely depending on the type of care.
In 2020, Mckinsey had estimated that the virtual enabled healthcare industry would become a $250 billion industry. Going by the recent trends the prediction is well and truly on course.
During the Pandemic the usage of Telehealth services surged as patients sought the safe access to seek virtual health services. Likewise for healthcare professionals it provided the luxury of discharging their duties without being on the frontline.
The Future Scenario:
During the outbreak of Ebola in 2015, workshops were organised by White House Office of Science & Technology Policy and the National Science Foundation broadly defined three areas where Robotics can make a significant difference. As a result, it set a precedence for handling Covid-19 pandemic.
• Clinical Care – Telemedicine & Decontamination
• Logistics – Delivery & handling of contaminated waste
• Reconnaissance – Monitoring Compliance
Covid-19 introduced a fourth area – contactless consultancy services. This opens up the future for Tele Health services with the possibility of remotely controlled robotic systems deployed to the frontline.
With 5G bandwidth and smart phones entering the public domain, the day won’t be far when Medical Conferences and seminars will be held virtually. As a result, this opens the door for virtual reality in the field of Medicine. Not only will such an initiative reduce infection rates, it will help in reducing carbon footprint as well.
During the pandemic, there has been an increase interest in decentralized and digitally connected rapid diagnostic tests to widen access to testing. As a result, this increase capacity and eases the strain on healthcare systems and diagnostic laboratories.
There is an urgent need for creating applications to predict future eventualities, availability of essential medical services and optimising medical resources. IT and IT based solutions is a force multiplier for the healthcare sector. The applications are efficient, fast and accurate. The other important aspect is that IT based solutions are cost effective. This makes healthcare accessible with virtual health services and reduces the burden on the Government and Hospitals. It is the future of medical services to meet the global demand of equitable healthcare.
Technology trends shaping the post Covid world:
Over a period of time, Artificial intelligence (AI) has evolved by leaps and bounds in detection, diagnosis, and treatment of diseases. In India, City Scan has helped in proof reading for Radiologist’s and reduced the time lapse for diagnosis. Similarly, eye testing etc. are widely using AI for faster diagnosis and treatment. Artificial Intelligence applications with proper implementation can address the global health care inequalities that exists today.
During Covid-19, Artificial Intelligence based technical models provided the following:
• Helped in reducing the response time to patients.
• Giving predictive models of mortality.
• Inventory management.
• Predictive model for scanning the wave of Covid-19.
• Predicting the end and resurgence of the wave.
Deep learning, a facet of machine learning, is based on artificial neural networks. It provides the healthcare industry with the ability to analyse data efficiently with pinpoint accuracy. It has the ability to reduce admin work and increase insights into the patient’s condition and requirements. This helps medical professionals to focus on their job – that is to save lives.
Along with AI and ML, Semantic analysis and Deep learning will be the buzz words in the medical field in the near future. Together they open up a possibility of transforming the sector altogether.
Digital technology can aid in the clinical research with symptom based case identification. During the Pandemic, online symptom reporting was done in Singapore and UK.
Final Thoughts:
With the global population going Tech Savvy, it has enabled virtual health business models to include a range of services. For eg: enabling longitudinal virtual care, integration of telehealth with other virtual health solutions, and hybrid virtual/in-person care models. It has the potential to improve consumer experience/convenience, access, outcomes, and affordability – Digital Healthcare is one for the future.
With increased awareness, the world is now more than ready to move from the norm and embrace the new.
Like other businesses, if you too are looking for IT Solutions for Healthcare Services, Mindfire Solutions can be your partner of choice. We have significant experience over the years working with Healthcare IT Companies. We have a team of highly skilled and certified software professionals, who have developed many custom virtual healthcare solutions for our global clients over the years.
Here are a few interesting projects we have done to develop virtual health solutions. Click here to know more: Case study on managing high risk patients.
Case study on PWA for mental health.